
Laser-Lok® microchannels
Improved as a result of more than 25 years of research, Laser-Lok technology provides an unparalleled surface treatment for BioHorizons implants and abutments that facilitates true, physical connective tissue connectivity.

Why is Laser-Lok unique?
Surface properties
The Laser-Lok is a series of cell-sized microchannels around the neck of the implant that are formed using a patented laser ablation technology. The microchannels created with this technology are extremely uniform and, due to their size (8 microns), greatly facilitate the alignment and attachment of osteoblasts and fibroblasts to the implant surface.15,16,17,18,19,20,21,22,23,24 The Laser-Lok microstructure also features a repetitive nanostructure that maximizes the available surface area and allows pseudopodia and microfibrils to intertwine with the Laser-Lok surface.
Other than traditional surface treatment
Most implants on the market today are sandblasted or acid etched. These manufacturing processes create an irregular, random surface that is different at every point. This also makes cell integration random.10 While these irregular surfaces integrate better than polished surfaces,11 only the Laser-Lok is able to properly attach both soft tissue and bone tissue to the implant.2,3,4,5,6,7,8,9,10
Lifetime warranty
All BioHorizons implants and prosthetics have a lifetime warranty. All BioHorizons implants and prosthetic elements can be replaced free of charge if the removal of the product is due to a defect (with the sole exception of the wear of the denture elements).
Opinions of recognized experts about Laser-Lok:
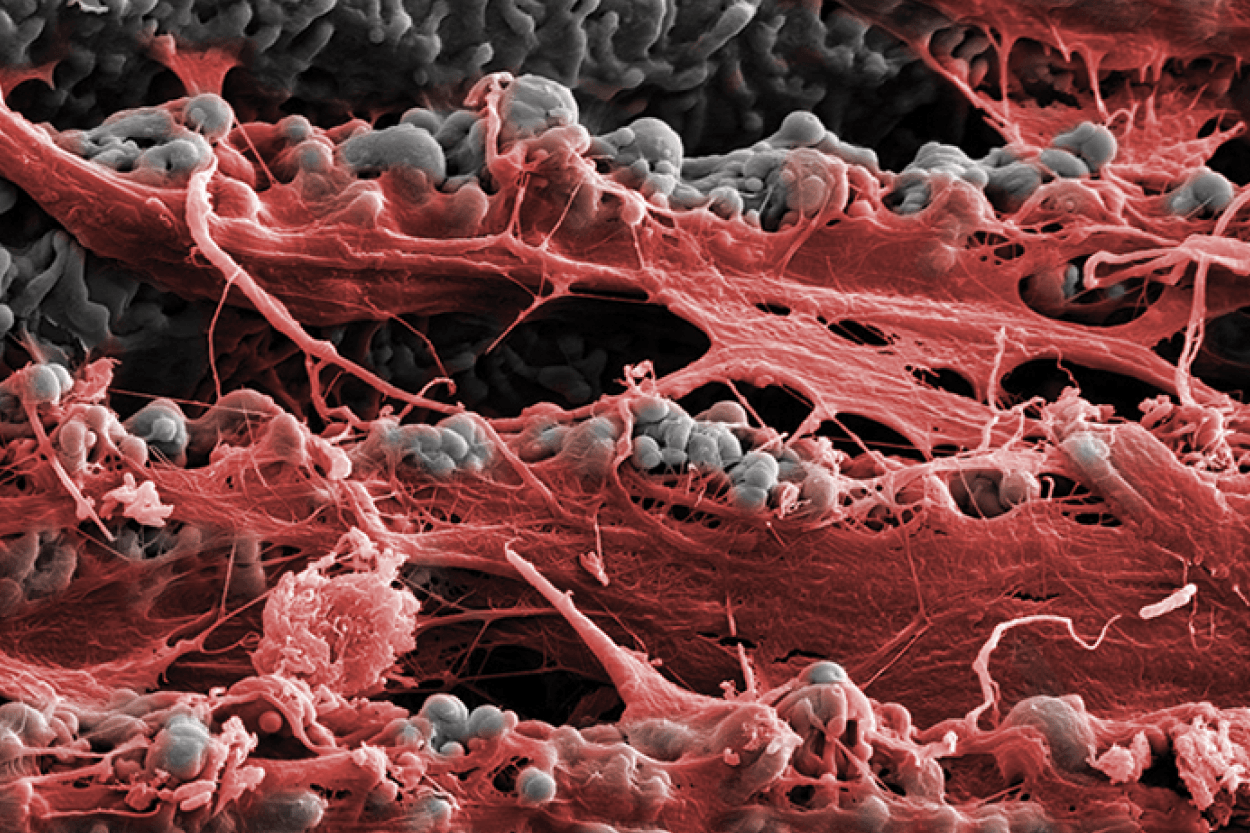
Tinted scanning electron microscope (SEM) image of soft tissue attached to the Laser-Lok surface.2


Key clinical benefits
Success rate
Predictable results
Implants with Laser-Lok surface treatment achieved a success rate of 100% in the anesthetic zone in 3 years27, in the most challenging regions for implantation.
Preservation of bone marrow

Preservation of bone marrow
Numerous studies have shown that the Laser-Lok surface has certain clinical advantages over other implants. A multicenter cohort study showed that when Laser-Lok implants were placed next to implants with a conventional surface, 37 months after surgery, bone loss at the Laser-Lok surface was reduced by 70% (by approximately 1.35 millimeters).11

Laser-Lok has been proven to reduce bone marrow loss by up to 70% compared to other conductive implants.13
Over a period of 3 years, bone loss can be reduced to up to 0.35mm.27
Outstanding results with immediate loading
Predictability is an essential condition for immediate loading. On average, Laser-Lok implants have a success rate of 97.2% at immediate load. Several studies on the immediate protocol have shown that implants with conventional surface treatment experience an average of 61% greater bone loss compared to Laser-Lok implants.28 Furthermore, Laser-Lok showed a higher bone-to-implant (BIC) ratio compared to conventional surfaces.14 After only 3 weeks, Laser-Lok implants have an average BIC of 51%. 29
Lower bag depth

One of the main causes of peri-implant disease and implant failure is increased sac depth.30 Laser-Lok surface treatment can reduce pouch depth by up to 1.21mm compared to other conductive implants.13
Reducing the chances of peri-implantitis

Reducing the chances of peri-implantitis
Confidence in every position

Confidence in every position
Whether implantation into the anterior or posterior regions, the mandible, or the maxilla, implants with Laser-Lok have an increased success rate and outstanding bone marrow retention for both immediate and delayed protocols.28
1. Implant success rate is the weighted average of all published human studies on BioHorizons implants. These studies are available for review in this document and BioHorizons document number ML0130.
2. Human Histologic Evidence of a Connective Tissue Attachment to a Dental Implant. M Nevins, ML Nevins, M Camelo, JL Boyesen, DM Kim International Journal of Periodontics & Restorative Dentistry. Vol. 28, No. 2, 2008.
3. The Effects of Laser Microtextured Collars Upon Crestal Bone Levels of Dental Implants. S Weiner, J Simon, DS Ehrenberg, B Zweig, JL Ricci. Implant Dentistry. Volume 17, Number 2, 2008. p. 217-228.
4. Influence of a microgrooved collar design on soft and hard tissue healing of immediate implantation in fresh extraction sites in dogs. SY Shin, DH Han. Clin. Oral Impl. Gap. 21, 2010; 804–814.
5. Maintaining inter-implant crestal bone height via a combined platformswitched, Laser-Lok® implant / abutment system: A proof-of-principle canine study. M Nevins, ML Nevins, L Gobbato, HJ Lee, CW Wang, DM Kim Int J Periodontics Restorative Dent. Volume 33, Number 3, 2013.
6. Histologic Evidence of a Connective Tissue Attachment to Laser Microgrooved Abutments: A Canine Study. M Nevins, DM Kim, SH Jun, K Guze, P Schupbach, ML Nevins. International Journal of Periodontics & Restorative Dentistry. Vol. 30, No. 3, 2010.
7. Histological evidence of connective tissue integration on laser microgrooved abutments in humans. NC Geurs, PJ Vassilopoulos, MS Reddy. Clinical Advances in Periodontics. Vol. 1, No. 1, May 2011.
8. Connective tissue attachment to laser microgrooved abutments: A human histologic case report. M Nevins, M Camelo, ML Nevins, P Schupbach, DM Kim Int J Periodontics Restorative Dent. Volume 32, Number 4, 2012. p. 384-392.
9. Reattachment of the connective tissue fibers to the laser microgrooved abutment surface. M Nevins, M Camelo, ML Nevins, P Schupbach, DM Kim Int J Periodontics Restorative Dent. Volume 32, Number 4, 2012. e131-134.
10. The impact of dis- / reconnection of laser microgrooved and machined implant abutments is soft- and hard-tissue healing. Iglhaut G, Becker K, Golubovic V, Schliephake H, Mihatovic I. Clin Oral Implants Res. 2013 Apr; 24 (4): 391-7.
11. Clinical Evaluation of Laser Microtexturing for Soft Tissue and Bone Attachment to Dental Implants. GE Pecora, R Ceccarelli, M Bonelli, H Alexander, JL Ricci. Implant Dent. 2009 Feb; 18 (1): 57-66.
12. Radiographic Analysis of Crestal Bone Levels on Laser-Lok® Collar Dental Implants. C Shapoff, B Lahey, P Wasserlauf, D Kim Int J Periodontics Restorative Dent. 2010; 30: 129-137.
13. The effects of laser microtexturing of the dental implant collar on crestal bone levels and peri-implant health. S Botos, H Yousef, B Zweig, R Flinton, and S Weiner. Int J Oral Maxillofac Implants. 2011; 26: 492-498.
14. Marginal Tissue Response to Different Implant Neck Design. HEK Bae, MK Chung, IH Cha, DH Han. J Korean Acad Prosthodont. 2008, Vol. 46, No. 6.
15. Osseointegration on metallic implant surfaces: effects of microgeometry and growth factor treatment. SR Frankel, J Simon, H Alexander, M Dennis, JL Ricci. J Biomed Mater Res. 2002; 63 (6): 706-13.
16. Connective-tissue responses to defined biomaterial surfaces. I. Growth of rat fibroblast and bone marrow cell colonies on microgrooved substrates. JL Ricci, JC Grew, H Alexander. Journal of Biomedical Materials Research Part A. 85A: 313-325, 2008.
17. Connective-tissue responses to defined biomaterial surfaces. II. Behavior of rat and mouse fibroblasts cultured on microgrooved substrates. JC Grew, JL Ricci, H Alexander. Journal of Biomedical Materials Research Part A. 85A: 326-335, 2008.
18. Interactions between MC3T3-E1 cells and textured Ti6Al4V surfaces. Soboyejo WO, Nemetski B, Allameh S, Marcantonio N, Mercer C, Ricci J. J Biomed Mater Res. 2002 Oct; 62 (1): 56-72.
19. Bone Response to Laser Microtextured Surfaces. JL Ricci, J Charvet, SR Frenkel, R Change, P Nadkarni, J Turner and H Alexander. Bone Engineering (editor: JE Davies). Chapter 25. Published by Em2 Inc., Toronto, Canada. 2000.
20. Cytoskeletal organization in three fibroblast variants cultured on micropatterned surfaces. JC Grew, JL Ricci. Presented at the Sixth World Biomaterials Congress. Kamuela, HI. May 15-20, 2000.
21. Cytological characteristics of 3T3 fibroblasts cultured on micropatterned substrates. JC Grew, SR Frenkel, E Goldwyn, T Herman, and JL Ricci. Presented at the 24th Annual Meeting of the Society for Biomaterials. April 22-26, 1998. San Diego, CA.
22. Effects of surface microgeometry on fibroblast shape and cytoskeleton. JC Grew, JL Ricci, AH Teitelbaum, JL Charvet. Presented at the 23rd Annual Meeting of the Society for Biomaterials. April 30-May 4, 1997. New Orleans, LA.
23. Cell interaction with microtextured surfaces. JL Ricci, R Rose, JK Charvet, H Alexander, CS Naiman. Presented at the Fifth World Biomaterials Congress. May 29-June 2, 1996. Toronto, Canada.
24. In vitro effects of surface roughness and controlled surface microgeometry on fibrous tissue cell colonization. JL Ricci, J Charvet, R Sealey, I Biton, WS Green, SA Stuchin, H Alexander. Presented at the 21st Annual Meeting of the Society for Biomaterials. March 18-22, 1995. San Francisco, CA.
25. Surface Topography Modulates Osteoblast Morphology. BD Boyan, Z Schwartz. Bone Engineering (editor: JE Davies). Chapter 21. Published by Em2 Inc., Toronto, Canada. 2000.
26. Effects of titanium surface topography on bone integration: a systematic review. A Wennerberg, T Albrektsson. Clin Oral Implants Res. 2009 Sep; 20 Suppl 4: 172-84.
27. Immediate versus delayed treatment in the anterior maxilla using single implants with a laser-microtextured collar: 3-year results of a case series on hard- and soft-tissue response and esthetics. Renzo Guarnieri, MD, DDS, Fabrizio Belleggia, DDS, & Maurizio Grande, DDS. Journal of Prosthodontics, Volume 25, Issue 2, February 2016. pp.135–145. 28.
28. The impact of laser microtexturing collar designs on crestal bone level, and clinical parameters under various placement and loading protocols. M Serra, L Bava, D Farronato, V Iorio Siciliano, M Grande, R Guarnieri. Int J Oral Maxillofac Implants 2014; 29: 354-363.
29. The effect of different surgical drilling procedures on full laser-etched microgrooves surface-treated implants: an experimental study in sheep Jimbo R, Tovar N, Yoo DY, Janal MN, Anchieta RB, Coelho PG. Clin Oral Implants Res. 2014 Sep; 25 (9): 1072-7.
30. Dental implants: Maintenance, care and treatment of peri-implant infection. Chen, S. and Darby, I. Australian Dental Journal, 48 (4), p. 212–220, 2003.
31. Microbiological findings and host response in patients with peri-implantitis. Hultin, M., Gustafsson, A., Hallstrom, H., Johansson, L., Ekfeldt, A., & Klinge, B. Clinical Oral Implants Research, 13 (4), 349-358, 2002.
32. Microbial Characteristics of Peri-Implantitis: A Case-Control Study. YC de Waal, HV Eijsbouts, EG Winkel, and AJ van Winkelhoff. February 2017, Vol. 88, No. 2, Pages 209-217.
33. A double-blind randomized trial comparing implants with laser-microtextured and machined collar surfaces: Microbiologic and clinical results. Guarnieri R, Rappelli G, Piemontese M, Procaccini M, Quaranta A. Int J Oral Maxillofac Implants. 2016; 31 (5): 1117-25.
34. Case provided by Dr. Cary Shapoff, DDS (Periodontist), and Dr. Jeffrey A. Babushkin, DDS (Restorative).
